
Allergic Rhinitis
Overview
Allergic rhinitis, often referred to as hay fever, is a common condition where the immune system reacts to environmental allergens like pollen, dust mites, or pet dander. Despite its name, hay is not the cause, and fever is not typically a symptom.
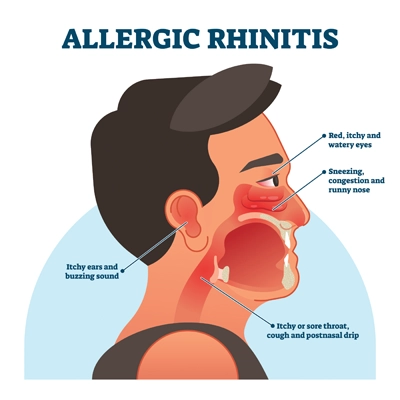
Common Symptoms
- Frequent sneezing
- Runny or blocked nose
- Itchy nose, eyes or throat
- Watery or red eyes
- Fatigue, especially if sleep is disrupted
Possible Triggers
- Airborne pollen (trees, grasses, weeds)
- Dust mites
- Animal fur or skin flakes (dander)
- Mould spores
- Changes in temperature or exposure to smoke
Self-Care and Prevention
While complete avoidance of allergens may not always be possible, the following steps may help reduce exposure:
- Keep windows closed during high pollen seasons
- Shower and change clothes after being outdoors
- Use a vacuum with a HEPA filter
- Wash bedding regularly in hot water
- Avoid smoking and minimise exposure to strong fragrances or chemicals
When to Seek Medical Advice
If symptoms persist or significantly affect your quality of life, it is recommended to speak with a qualified healthcare professional. They can help identify possible triggers and discuss suitable management options.
