
Blood Clots
Understanding Circulatory Health and Blood Flow Awareness
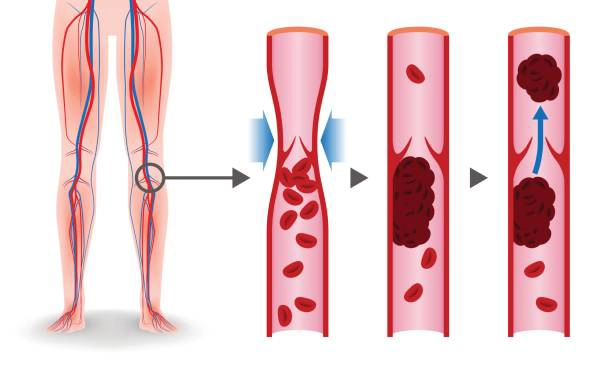
The body’s ability to manage blood flow and healing is one of its most remarkable systems. When an injury occurs, the body responds by forming a temporary barrier at the site—this is part of a natural process that helps limit blood loss and support recovery.
However, in some cases, changes in blood circulation can affect how we feel. Being informed about what may influence blood flow and vessel health can help you better understand your body and when to reach out to a healthcare provider for support.
How the Body Responds to Injury
When we sustain a cut or internal injury, the body responds in several coordinated ways:
- Vessel Tightening (Vasoconstriction): The blood vessels naturally narrow around the injured area to reduce blood loss.
- Platelet Activity: Platelets (a type of blood cell) gather at the injury site to help form a temporary plug.
- Protective Proteins: Specialised proteins in the bloodstream support the development of a mesh-like structure to help seal the injury and support healing.
What May Affect Healthy Circulation
There are a variety of factors that may influence how blood circulates through the body, including:
- Long periods of physical inactivity (e.g., long flights or bed rest)
- Ageing and natural changes in blood vessels
- Lifestyle factors such as smoking or poor diet
- Family history and inherited traits
- Hormonal changes or certain medications
- General inflammation or long-term health conditions
Looking After Circulatory Health
Supporting healthy blood flow and vascular wellbeing is something we can often work toward through everyday choices. Here are a few general habits that may contribute to better circulatory health:
1. Stay Active
Regular movement helps encourage healthy circulation. Activities like walking, stretching, or swimming can help support overall wellbeing.
2. Take Breaks During Long Periods of Sitting
Whether you're working at a desk or travelling, taking a moment to stand and stretch can support healthy blood flow.
3. Eat a Balanced Diet
Including whole foods such as vegetables, fruits, whole grains, and healthy fats may contribute to better cardiovascular function.
4. Stay Hydrated
Drinking enough water throughout the day can support healthy circulation and energy levels.
5. Speak with a Healthcare Professional
If you have a family history of circulatory conditions, or if you’re unsure about your personal risk factors, it's always a good idea to check in with a qualified health provider.
When to Seek Support
If you ever notice unexplained swelling, pain, or other unusual symptoms, don’t delay seeking medical advice. While not all symptoms relate to blood circulation, only a qualified healthcare professional can assess and guide you based on your individual health needs.
Prime Medic offers non-urgent telehealth consultations with registered healthcare professionals. If you have general concerns about your wellbeing, you can book an online appointment from the comfort of your home.
